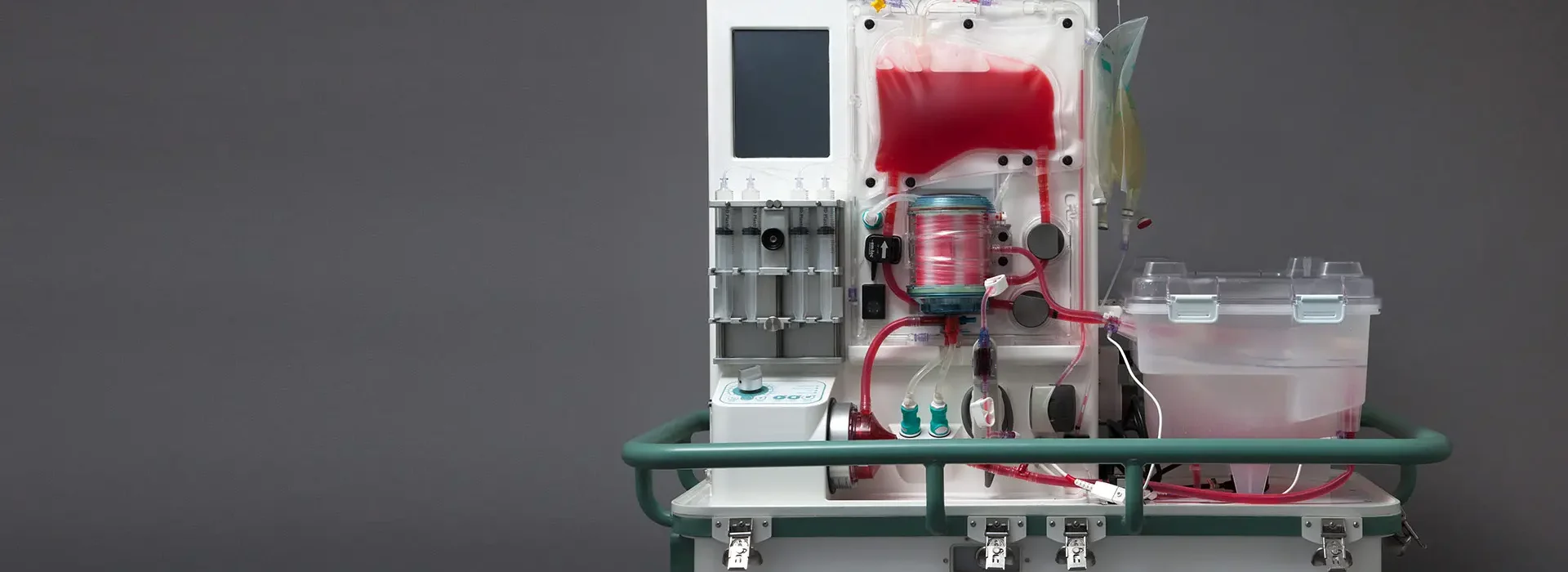
A world-first system that keeps transplant livers alive
Challenge
Transforming a large, manual process into an automated, transportable liver perfusion device.
Approach
Combining expertise from across all our disciplines, we developed a small system suitable for commercial use and transport from the original manual lab-based system.
Outcome
Following the delivery of a proof-of-principle device, we took the system through to successful use in clinical trials. This device can now preserve livers for up to 24 hours before transplantation and provide real-time data which the physician can use to assess liver viability. The metra® is now a multi award-winning commercially available product.